Navigation:
Introduction & Summary
Narrative Review:
—[Congenital Heart Disease]
—[Homosexuality]
—[Left Handedness]
—[Autoimmune Disorders (Cœliac, Crohn’s, & Inflammatory Bowel Diseases, etc)]
—[Hypothyroidism]
—[Lupus]
—[COPD & Chronic Respiratory Diseases]
—[Parkinsonism, Alzheimer’s Disease, & Dementia]
—[Multiple Sclerosis]
—[Sleep Apnea]
—[Cancers]
—[Impulse Control]
—[Blood Pressure, Diabetes, Cardiovascular Health, & Obesity]
—[Bipolar Disorder]
—[Depression]
—[Autism]
—[Neuromuscular Disease]
—[Peripheral Artery Disease]
—[Sarcoidosis]
—[Dry-Eye Disease]
—[Chronic Fatigue Syndrome]
—[Fibromyalgia & Chronic Widespread Pain]
—[Periodontal Health]
—[Leprosy]
—[Arthritis, Renal Disease, & Miscellaneous Age-Associated Diseases]
—[Symptomatic Kidney Stone Disease]
The Global Burden Of Disease Dataset:
—[Main Categories]
—[All Categories]
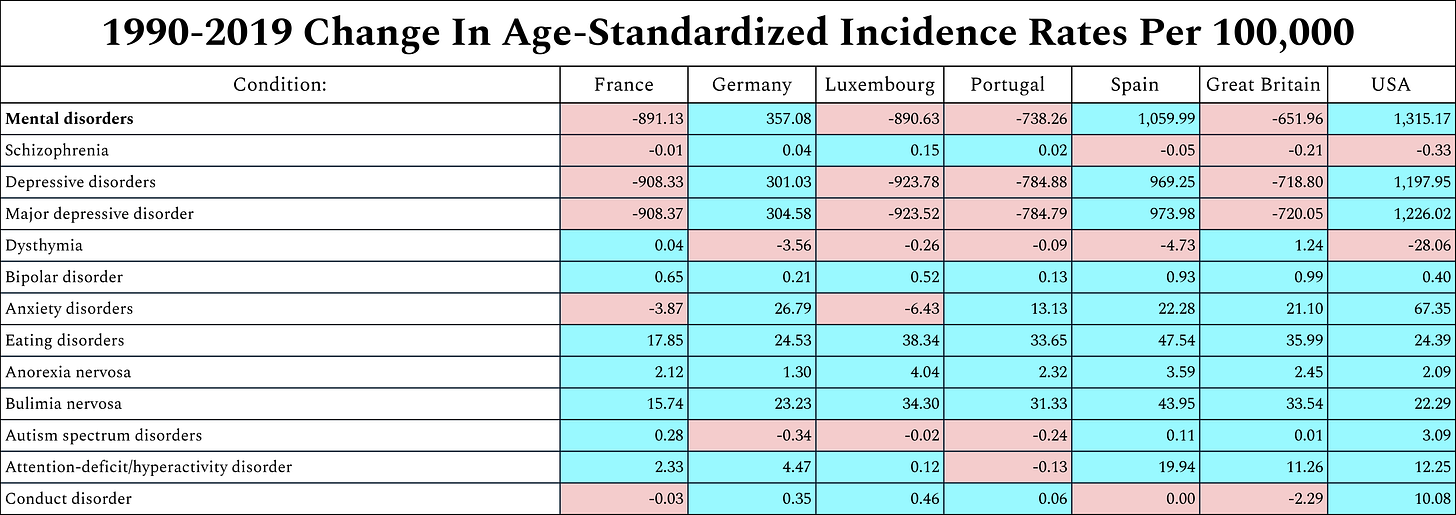
—[Mental Disorders]
—[Neurological Disorders]
—[Congenital Birth Defects]
—[Neoplasms (i.e. Cancers)]
—[Cardiovascular Diseases]
—[Chronic Respiratory Diseases]
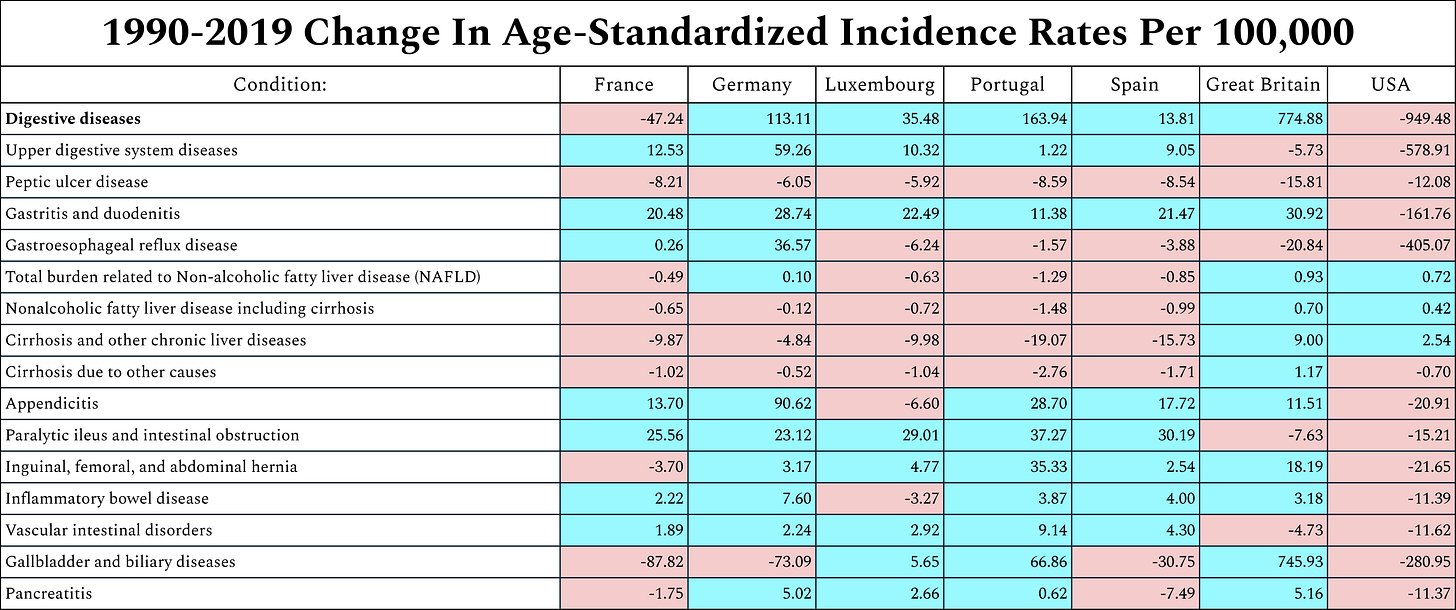
—[Digestive Diseases]
—[Diabetes & Kidney Diseases]
—[Skin & Subcutaneous Diseases]
—[Musculoskeletal Disorders]
—[Other Non-Communicable Diseases]
—[Communicable, Maternal, Neonatal, & Nutritional Diseases]
References
Introduction & Summary:
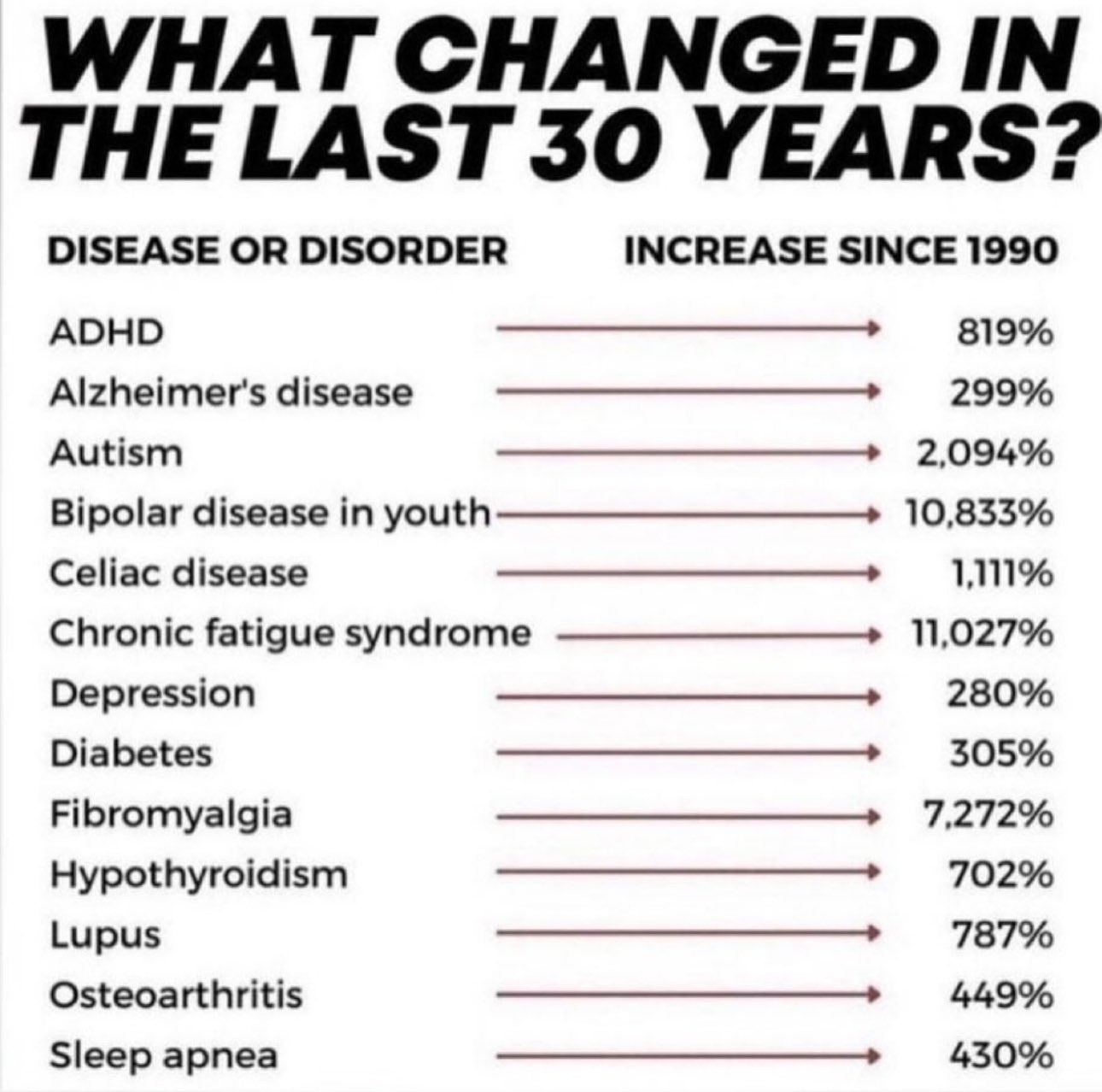
Recently on twitter I saw somebody post the following (unsourced) graph [1]:
It got about the reaction I was expecting [2]:
In principle, one could remark that “what’s asserted without evidence can be dismissed without evidence”, but this is an argument that’s been pursued before with a greater degree of rigor, albeit for a different set of outcomes [3]:
In practice then, dismissing these claims without evidence is more akin to denying the rarity of pedophilia:
For any given aspect of declining health, one can always produce no end of speculation as to possible environmental reasons that it might be happening. However, if declines are happening everywhere, then this requires that causes be posited which are of greater ætiological generality. This is the strength of an explanation which attributes declines to mutation (i.e. generalized declines in genetic quality within the population). Randomly-generated sequences of DNA generally do not code for anything. Most possible strings of DNA would produce nothing but a useless pile of goo. As such, mutation should be understood as genetic entropy. As the story goes, since industrialization and modern medicine have eliminated infant mortality, this is to be understood as a partial abolition of the Malthusian selection pressures which were once a check against this genetic entropy, and so one might expect generalized declines in genetic health as a result.
Alternatively, if other causes of similar ætiological generality can be shown to be explanatory, or if the premise of general declines in health are false to begin with, then one need not worry so much. I propose two alternative explanations possessing the same ætiological generality:
As fertility has collapsed and life expectancy has increased, the population pyramids of industrialized nations have come to look like this [4, figure 2.A]:
Given that the elderly tend to be less generally healthy than the young, one should expect declines across the board simply due to aging populations. It is entirely possible for overall disease prevalence to rise even as age-standardized disease prevalence declines.
There is a difference between disease prevalence and disease incidence. Western health systems are generally becoming better with time, and the consequence of this is that as the mortality rate of a disease declines, the people afflicted by it can become a larger percentage of the population even as the yearly rate of new cases declines. Ideally, we should want to verify systemic rises in age-standardized disease incidence.
In addition to these factors, there’s also the problem of there being hundreds of ailments somebody can be afflicted with, meaning that there’s a need to try to study a large, unbiased selection of them, and to rely upon a comprehensive selection of the evidence that exists on any one of them. Generally speaking, rather than limiting ourselves to any one country, we also care about any region of the world that happens to be inhabited by people of Nordic or Western-European ancestry.
To accomplish all of these goals, I take two approaches:
First, on google scholar, I search the following along with a couple of analogous searches up to about page 10 or so, or just when I got tired:
(disease OR anemia OR disorder OR pathology) AND "incidence" AND ("over time" OR trends OR "trends in" OR "trend in" OR "time-series" OR "time series" OR "increase in") AND (developed OR industrialized OR OECD OR Europe OR "United States" OR "North America")
If a particular ailment kept coming up and drowning out other results, I’d modify searches to exclude it and mark it as something to look into individually (i.e. I’d repeat the search again but replacing “(disease OR anemia OR disorder OR pathology)” with whatever excluded ailment). In addition to manually-excluded ailments, I’d also pay individual attention to every disorder on the meme graph, every disorder from Bronski’s list, and a couple of miscellaneous conditions I’d happened to think of which had evidence readily available.
If I could only find information on prevalence, then if it was stable or declining, I considered this prima-facie evidence against an increase in age-standardized incidence. The same goes for age-standardized prevalence and for raw incidence, whatever the most rigorous available standard happened to be. If increases were evident for age-standardized incidence, this was considered prima-facie support for a mutational-load view. There weren’t many of these however, and when they occurred, I took the liberty to see if some other explanation could be confirmed, whether this be changes in measurement, an environmental origin of the rise, etc. In summary, there are very few ailments seeing a rise in age-standardized incidence which could possibly be consistent with a mutational-load explanation, and the stability or decline in everything else contradicts the view that a mutational-load explanation is advantaged by its ætiological generality.Second, I use the 1990-2019 Global Burden of Disease Study [5], which tabulates yearly data for the 337 leading ‘causes of death’ across 188 nations. Specifically, I look at changes from 1990 to 2019 in age-standardized incidence rates for 261 relevant ailments (i.e. excluding things like physical injuries) for which there is data within 7 nations of interest: The United States of America, Great Britain, France, Germany, Luxembourg, Spain, and Portugal.
The United States is the country with the highest White population, Portugal is the Western-European country with the most-dysgenic fertility [6], Luxembourg has Europe’s highest per-capita GDP and lowest infant mortality rate [7] (excluding Monoco, a city state having a below-100k population which causes problems for calculating per-100k incidence rates), Germany is the most industrialized country in Europe, accounting for 26% of European production capacity [8], France was the first country in the world to undergo the fertility transition [9, figure 1], England was the first nation in the world to industrialize [10, ch.12-13], and Spain is the Western-European country with the lowest fertility rate [11].
Broadly, I find that outcomes are evenly split between age-standardized incidence rates rising and declining, even for the categories of highest theoretical relevance (these being mental disorders, neurological disorders, congenital birth defects, and neoplasms i.e. cancers). The headline results are as follows:In addition to the analyses presented here, some day I’d also like to also factor analyze the between-nations variation in all ailments to see what the different dimensions of health are, and to come up with a dimension of general (especially ‘innate’) health before employing latent growth modelling to see if the changes can be predicted by national-level differences in dysgenics and in infant mortality, controlling for national IQ and per-capita GDP. As it stands however, the analyses I present today took long enough, and I’ll only do a part 2 if this initial post generates enough paid subscriptions to justify the required time investment.
Narrative Review
Congenital Heart Disease:
The global prevalence of congenital heart disease has increased from 0.6 per 1000 in 1930 to 9.1 per 1000 after 1995, which is important because CHD accounts for nearly one-third of all major congenital anomalies [12]. This cannot be blamed on third-world fertility as it has also increased within china, from 0.201% in 1980-1984 to 4.905% in 2015-2019 [13]. One might suspect that it's a rise in prevalence rather than incidence though, as mortality for the condition has decreased by 31% between 1987 and 2005 [14], but this is implausible since it's birth prevalence being measured. While the example of congenital heart disease is probably one of the best things that a mutational-load account has going for it, the trend has stagnated from 1990-2017 [15]; in central europe, western europe, north america, and australia, the percent change in prevalence at birth over this time period was -0.4%, +18.2%, -0.3%, and +0.5% respectively. For low, low-middle, middle, high-middle, and high SDI countries, the percent changes over this time period was -0.6%, -1.6%, -2.4%, -1.9%, and 0.6% respectively [15].
Homosexuality:
The rise in homosexuality is real and not completely attributable to rises in tolerance, albeit it's mostly a rise in bisexuality, one stronger among women then men, as one might predict if, instead of tastes changing, increasing proportions of the 'sexually fluid' merely began expressing their diverse tastes [16].
Left Handedness:
A k=262 meta-analysis found no significant correlation between publication year and percent left handed [17].
Autoimmune Disorders:
(Cœliac Disease, Crohn’s Disease, Inflammatory Bowel Disease, etc)
Autoimmune disorders within industrialized nations are (mostly) increasing, but we have strong evidence that the rise is environmental in origin. First let’s take note of the evidence for rising incidence:
[18] A systemic review of studies from 1985 to 2015 found rheumatic, endocrinological, gastrointestinal, and neurological autoimmune diseases to have annual increases of 7.1%, 6.3%, 6.2%, and 3.7% respectively.
[19] An N = 22,009,375 UK cohort study found a significant change in the proportion of people with at least one autoimmune disorder (IRR = 1.04), with the growth being especially large for Cœliac disease (IRR = 2.19), Sjogren's syndrome (IRR = 2.09), and Graves' disease (IRR = 2.07), although Pernicious Anaemia (IRR = 0.79) and Hashimoto's thyroiditis (IRR = 0.81) showed decreased incidence.
[20] As the meme graph claims, this meta-analysis finds that the age-standardized incidence Cœliac disease has unambiguously increased more than 10-fold since 1980.
[21] This systemic review from 1985-2018 found an increase in the incidence of pædiatric-onset inflammatory bowel disease.
[22] Interestingly enough, this meta-analysis found no increase in the incidence of Crohn's disease (i.e. one of the major types of IBD).
[23] This representative UK study found a decrease in the incidence of dermatitis herpetiformis from 1990 to 2011.
[24] In 20-29 year old women within industrialized nations, this paper found an increase in incidence of pelvic inflammatory disease between 1960 and 1980 on the order of a factor of 1.6-1.9.
Now how do we know that the rise is environmental in origin? Well, studies of immigrant groups moving to different nations find that autoimmunity changes to reflect that of host populations [21, p.2742; & 25, p.912], and this works both for high-autoimmunity groups moving to low-autoimmunity areas (e.g. Pakistanis moving to the UK) and for low-autoimmunity groups moving to high-autoimmunity areas (e.g. Englishmen moving to Australia). Looks like magic dirt theory isn’t so silly in this case. Moreover, we have a good idea of the mechanism. The primary defect shared by people with autoimmune diseases is a dysfunction of TJ (intestinal tight junction) regulation, and there's a strong case that various additives within industrially processed foods induce intestinal permeability, with consumption of these additives having steeply risen over time [26]. Animal experimentation studies feeding mice the same ingredients also find such diets to result in autoimmune diseases [27, p.7], although interestingly, not in bacteria-free conditions, thereby suggesting that microbiome disruptions are the mechanism by which these ingredients cause TJ defects. Do the animal studies generalize? Well, we have two meta-analyses of experiments finding that autoimmune disease remission can be induced either by administering priobiotics and synbiotics [28], or by transplanting fæcal matter from healthy people to patients with autoimmune disorders [29].
Hypothyroidism:
A meta-analysis found that between 1969 and 2020, the incidence of congenital hypothyroidism at birth increased in Europe from 2.32 per 10,000 to 3.73 per 10,000, and in high-income countries from 2.37 per 10,000 to 3.59 per 10,000; increases also were not attributable to changes in screening [33]. Hypothyroidism is another autoimmune disorder however. One might suspect that like other autoimmune disorders, the increase in incidence of congenital hypothyroidism might be due to increased consumption of additives in processed foods. Indeed, when cases due to dyshormonogenesis are excluded, immigrant groups moving to foreign countries adopt the disease rates of their new environments [34]. However, a nationwide, multicenter French analysis found not only that there was an increase in the incidence of congenital hypothyroidism which wasn't attributable to diognistic changes, but the increase was exclusive to cases of dyshormonogenesis (i.e. cases attributable to inborn errors in the eutopic glands responsible for thyroid hormone synthesis rather than cases attributable to problems in embryonic development) [35]. Indeed, other studies have found that cases due to dyshormonogenesis have risen to account for 30% of cases of hypothyroidism, as opposed to the prior proportion of 15% [36, p.5].
Hypothyroidism is probably the single most appealing case for an ML account of health declines. A review of twin studies found liability for thyroid disease to have a heritability of ~75% [37]. Another study found that patients with congenital hypothyroidism had a high frequency of mutations within candidate genes for dyshormonogenesis [38]. Contrary to most autoimmune disorders, the emergence of hypothyroidism is probably genetic in origin. However, even if something is increasing for genetic reasons, this does not necessarily imply that it is increasing due to mutation.
One alternative explanation to offer is immigration. In New Zealand, the incidence of congenital hypothyroidism has been increasing, but this is exclusively due to Asians and Pacific Islanders becoming larger proportions of the population; race-specific rates remained constant [39]. In the United States as well, it’s also arguably true that the growth in congenital hypothyroidism is entirely driven by Hispanic immigration [40]. At the national level, no ethnic group had any change with p<0.01, and arguably, with a multiple testing correction, Whites wouldn't even be p<0.05 either [40, table 2]:
When all states are put together, this restricts the range of time for which data is available, but within-state analyses of Texas and Massachusetts give further reason to doubt any increase among Whites. Massachusetts is one of the Whitest (>90%) and highest-latitude states in the union, and correcting for birth weight (a primary risk factor for congenital hypothyroidism at birth, with cases of this ætiology being imperative to ignore since they naturally cure themselves with age), the incidence trends in Massachusetts look like this [40, figure 9]:
In Texas, the incidence rate for non-Hispanic White boys increased while the incidence rate for non-Hispanic White girls decreased, such that the overall trend was a significant decrease [40, p.S44]. There was a significant within-Mestizo increase, but A) Mestizos aren’t a group we care about; and B) Mestizo immigrants to the United States have been increasing in Amerindian ancestry since the 1940s [41].
Immigration explanations however work less well for locations like France [35], Québec [42], Ireland [43], and other areas of Europe with known increases [44]. Still, the fact that genetic increases in hypothyroidism aren't omnipresent within wealthy western European populations is a problem for a Mutational-Load account of decline. Why the differences? Well, there's another way that genetic propensities can change without mutational pressure: selection. A recent meta-analysis found pediatric patients with hypothyroidism to score 10.48 IQ points lower than controls [45]. Of course, with more-educated women having children later in life, dysgenic selection for intelligence is pervasive throughout the world [6]. If selection against hypothyroidism is a consequence of selection for intelligence, one might also expect selection against intelligence to result in rises in hypothyroidism. Are the European rises in hypothyroidism also happening in the countries with less-dysgenic fertility? Finland is the 5th-least dysgenic nation on the planet [6], and as it turns out, large, representative cohort studies in Finland have found the incidence of hypothyroidism to be the same in 2017 as in 1994 [46].
Lupus:
A systemic review of studies on the incidence of lupus [50] found that incidence decreased in the UK from 1999 to 2012 (this is in spite of prevalence in the UK increasing over the same time period), decreased in the USA from 1980 to 2005, increased in denmark from 1980 to 1994, increased in greece from 1982 to 2001, and increased in the USA from 1950 to 1992. Lupus is also an autoimmune disorder, so we'd expect similar rises for the same environmental reasons we see rises in the other autoimmune diseases.
COPD & Chronic Respiratory Diseases:
Due to a decrease in the mortality of the disease, this Québec cohort study found that Chronic Obstructive Pulmonary Disease (COPD) has decreased in age-standardized incidence from 2001-2011 despite increasing in age-standardized prevalence over the same time period [30]. When prevalence isn’t standardized to a constrant age distribution across time periods, the prevalence increase is also substantially inflated [31]. Another study using the global burden disease also aligns with my analysis, finding that despite increasing prevalence, trends in most chronic respiratory diseases are not cause for concern within high-SDI countries [32, fig.4]:
Parkinsonism, Alzheimer’s Disease, & Dementia:
The incidence of Dementia has been decreasing while the incidence of Alzheimer’s Disease has remained steady in the West, although the incidence of Alzheimer’s has been increasing in non-Western countries [47 & 48]. As for Parkinsonism, incidence among Americans has increased, but only for men [49].
Multiple Sclerosis:
The numbers in my analysis of the GBD study are a complete nonsense due to what has to be a coding error (incidence rates above 500k per 100k). By contrast, in this systemic review [51], when looking at representative samples with consistent measures of multiple sclerosis, there was no evident pattern of MS incidence increasing; of these 3/9 studies finding an increase, two were Canadian and thus redundant, and the third was in Taiwan, a country of non-interest. Even these Canadian results might plausibly be attributed to the country's aging population, as in the Canadian study with measures of pædiatric-onset multiple sclerosis which were consistent across time, no change in incidence was evident.
Sleep Apnea:
The rise in sleep apnea is real. I couldn't find any other evidence to go on, but in the US, age-specific incidence rates in the military increased between 2005 and 2014 [52].
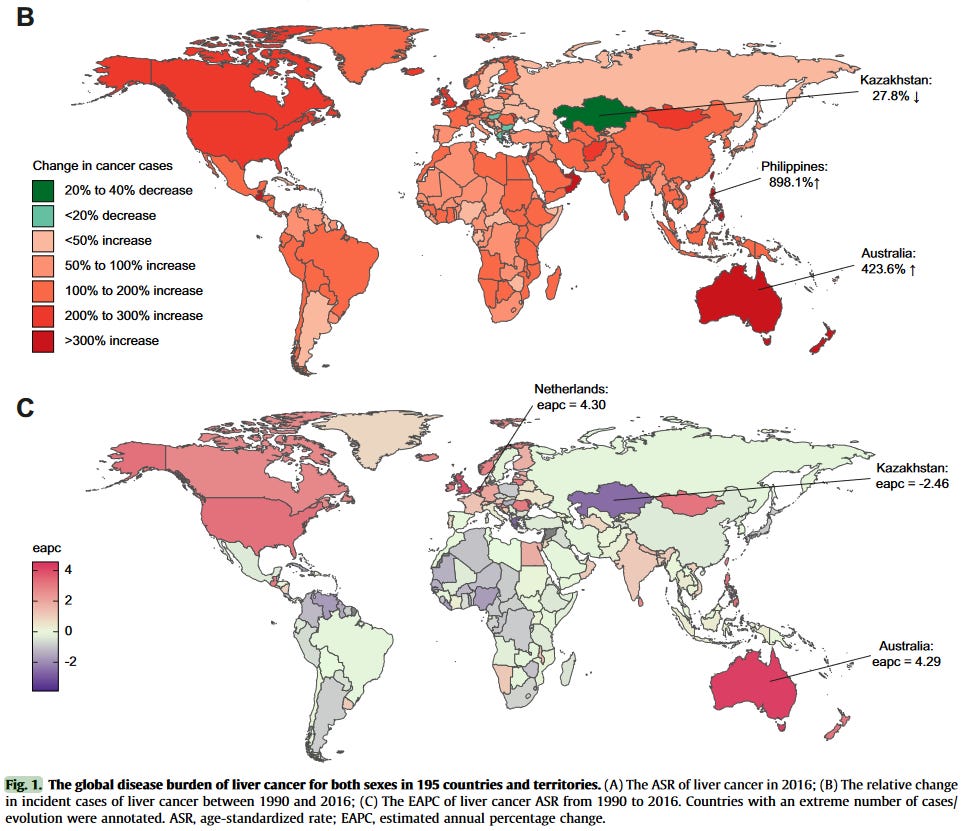
Cancers:
There are many different types of cancer, and as is evident from my analysis of the Global Burden of Disease dataset, whether or not incidence rates are increasing depends on the type of cancer. I didn’t bother to check too many of these, but a few types we might consider of particular interest to mutational-load theory are those which affect the reproductive systems of men and women; these seem to be declining:
[53] Between 1970 and 2015, industrialized nations have seen no obvious pervasive increases in the age-standardized incidence of ovarian cancer.
[54 & 55] Penile cancer incidence in the USA decreased from 1973-2002 [54] before stagnating from 2000-2014 [55].
[56] This paper found that the incidence of colorectal cancer in the United States decreased from 54.5 in 2000 to 38.6 per 100,000 in 2014.
[57] This paper found that from 1976 to 2005, the age-adjusted incidence of proximal colon, distal colon, and rectal cancers per 100,000 population in the US decreased from 22.5, 18.8, and 19.2 to 21.1, 11.7, and 13.6, respectively.
[58] This CDC report found age-adjusted melanoma incidence in the US to have doubled from 1982 to 2011.
[59] This GBD study paper found large age-standardized increases in the incidence of primary liver cancer from 1990 to 2016 which were particularly large within high-SDI countries [59, fig 1.b & fig 1.c]:
[60, table 1] Lip and oral cavity cancer incidence has increased all over the world except for high-SDI countries where it has decreased. Nasopharnygeal cancer incidence has decreased everywhere, and other pharyngeal cancer incidence has increased everywhere.
The United States is the nation where we have the most comprehensive cancer data, and since 1975, the “Annual Report to the Nation on the Status of Cancer” has documented a sustained decline in the overall age-standardized cancer incidence [100].
Impulse Control:
It may surprise many to learn that impulse control among children has been increasing over the past 50 years [61]. This arguably also seems to be reflected in many aspects of youth behavior. Traditionally, it’s been understood that there’s a relationship between age and crime, with younger people committing more offenses; recently however, the age-crime curve has been weakening [62]. Young people are also drinking and smoking less these days [63 & 64] and having less casual sex [65 & 66].
Blood Pressure, Diabetes, Cardiovascular Health, & Obesity:
Diabetes has been rising around the world. A systemic review [81] found that age-specific incidence rates of type-2 diabetes had been increasing throughout the industrialized world until around 2000, after which incidence started decreasing everywhere except for Denmark and Germany. The GBD dataset by contrast found widespread persistent increases.
A meta-analysis of RCTs finds that cardiovascular health is improved by drugs which lower blood pressure, with effects not moderated by type of drug [67]. High blood pressure is also a primary risk factor for diabetes [87], and there is strong evidence that obesity is causal for higher blood pressure [88 & 89]. The obese have 7.19 times the relative risk of developing diabetes [90], and the association remains even among people with normal metabolic health [91].
How have each of these things been changing over time? BMI increased persistently in Great Britain and in the United States between 1930 and 2000 [92] before stagnating in the United states from 2003 to 2012 [93]. Obesity in Sweden also increased between 1960 and 2010 [94], and a meta-analysis found that childhood obesity increased in Europe between 1999 and 2016 [95]. As we might expect from this, diabetes has been rising around the world. A systemic review [81] found that age-specific incidence rates of type-2 diabetes had been increasing throughout the industrialized world until around 2000, after which incidence started decreasing everywhere except for Denmark and Germany; the GBD dataset by contrast found widespread persistent increases. How about blood pressure and cardiovascular health? As it turns out, another meta-analysis finds that if anything, blood pressure among children has been decreasing despite the increase in obesity [68]. Another US study tracking trends in cardiovascular health metrics among adults found that although BMI and blood glucose had increased between 1988 and 2010 while physical activity decreased over the same period, blood pressure and cholesterol levels had decreased concurrently [98]. As for cardiovascular diseases, in the Global Burden of Desease dataset, age-standardized incidences of cardiovascular diseases were also down across the board between 1990 and 2019, and the other evidence I’ve been able to find on this question [96 & 97] is consistent with the GBD results.
So, it would seem that some decline in health is apparent in terms of obesity and in terms of diabetes, but not in terms of blood pressure or cardiovascular diseases. Suppose we were to just ignore the latter two. Should increased obesity be expected to lead to a rise in left-wing views? The best paper I know of found that controlling for poverty, spatial autocorrelation (!), racial demographics (!), and educational attainment, US counties with more obesity were more likely to vote for Romney in 2012 [99].
Bipolar Disorder:
Contrary to my results from the GBD dataset, this meta-analysis found no change in the age-standardized prevalence of bipolar disorder between 1990 and 2013 [69]. This may not be too unexpected given how small the increase in the BDP datset was to begin with.
Depression:
A 2018 meta-analysis found that the 1964-2015 increase in anxiety, depression, and neuroticism is exclusive only to the united states and did not occur in Europe [70]. This is consistent with the results from my analysis of the GBD dataset. This European stability is pervasive across many countries. One WHO-dataset analysis finds the following for age-standardized suicide mortality [71, fig.1]:
The longest-running suicide dataset we have comes from England and Wales, where the trend in age-standardized suicide mortality is as follows [72, figure 1]:
Autism:
Autism diagnoses are rising, but this is due to changes in measurement [73].
Neuromuscular Disease:
From 2003-2014 in Canada, neuromuscular disease incidence remained stable among children and decreased by 3% among adults [74].
Peripheral Artery Disease:
Peripheral Artery Disease incidence in the UK has decreased from 2000 to 2014 [75].
Sarcoidosis:
A representative US sample found an increase in the prevalence of sarcoidosis in the US, which cannot plausibly be attributed to age since the trend was constant across the age distribution [76, fig.3]. The GBD-dataset results also show increases in incidence.
Dry-Eye Disease:
From 2003 through 2015, Americans have seen age-specific increases in the incidence of dry eye disease [77].
Chronic Fatigue Syndrome:
I didn’t find any studies analyzing incidence (or even prevalence) by cohort and the GBD dataset didn’t have any information either. I found a meta-analysis [78] however that gives CFS incidence rates by publication year but does not analyze trends over time. I checked myself, and when weighing observations by squared reciprocal standard errors, there is an insignificant negative correlation of r = -0.006831783 between publication date and incidence rate.
Fibromyalgia & Chronic Widespread Pain:
Fibromyalgia is a disorder characterized by chronic widespread musculoskeletal pain. I didn’t find any studies analyzing trends in fibromyalgia, and it isn’t in the GBD database either, but I did find a meta-analysis [79] of the prevalence of chronic widespread pain which gives prevalence rates by publication year without analyzing trends over time. Weighing by squared reciprocal standard errors, there was a correlation of r = -0.7444931 between publication year and prevalence rate.
Periodontal Health:
In Sweden, the proportion of periodontally-healthy individuals increased from 8% in 1974 to 44% in 2003 [80].
Leprosy:
A CDC report [82] found the incidence of leprosy in the United States to be stable between 1994 and 2011, and found and that immigrant groups converge over time to the native rate.
Non-Alcoholic Fatty Liver Disease:
A meta-analysis [83] found no evident increase in the prevalence of Non-Alcoholic Fatty Liver Disease over time.
Arthritis, Renal Disease, & Miscellaneous Age-Associated Diseases:
While trying to find information on trends in the incidence in Arthritis and in Renal Disease, I came across a paper [84] using Medicare data in the National Long Term Care Survey to look at age-specific changes in a wide variety of age-related diseases. The results section speaks for itself:
Increases of incidence rates were dramatic for renal disease [the average annual percent change (APC) is 8.56%, 95% CI = 7.62, 9.50%], goiter (APC = 6.67%, 95% CI = 5, 90, 7, 44%), melanoma (APC = 6.15%, 95% CI = 4.31, 8.02%) and Alzheimer’s disease (APC = 3.96%, 95% CI = 2.67, 5.26%), and less prominent for diabetes and lung cancer. Decreases of incidence rates were remarkable for angina pectoris (APC = −6.17%, 95% CI = −6.96, −5.38%); chronic obstructive pulmonary disease (APC = −5.14%, 95% CI = −6.78,−3.47%), and ulcer (APC = −5.82%, 95% CI = −6.77, −4.86%) and less dramatic for carcinomas of colon and prostate, stroke, hip fracture and asthma. Incidence rates of female breast carcinoma, myocardial infarction, Parkinson’s disease and rheumatoid arthritis were almost stable.
Another paper on secular trends in the incidence of Rheumatoid Arthritis found that it did not change from 1995 to 2014 in California [85].
Symptomatic Kidney Stone Disease:
Symptomatic kindey stone disease incidence has not increased in iceland, although asymptomatic case detection has increased due to improved imaging [86].
The Global Burden Of Disease Dataset:
Cells show 2019 incidence rates subtracted from 1990 incidence rates (i.e. red cells indicate declining incidence over time):
Main Categories:
All Categories:
Mental Disorders:
Neurological Disorders:
Congenital Birth Defects:
Neoplasms (i.e. Cancers):
Cardiovascular Diseases:
Chronic Respiratory Diseases:
Digestive Diseases:
Diabetes & Kidney Diseases:
Skin & Subcutaneous Diseases:
Musculoskeletal Disorders:
Other Non-Communicable Diseases:
Communicable, Maternal, Neonatal, & Nutritional Diseases:
References
https://twitter.com/jaco_davidson/status/1785173107851808774
Bronski, J. (2023). Decline in Conservatism Between Generations Correlates Highly with Potential Signals of Mutational Load. Joseph Bronski Substack. Retrieved from https://www.josephbronski.com/p/decline-in-conservatism-between-generations
Vos, T., Barber, R. M., Bell, B., Bertozzi-Villa, A., Biryukov, S., Bolliger, I., … Dicker, D. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 386(9995), 743–800. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/S0140-6736(15)60692-4
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Cause-Specific Mortality 1990-2019. Seattle, United States of America: Institute for Health Metrics and Evaluation (IHME), 2024. Queryable at https://vizhub.healthdata.org/gbd-results/
Jensen, S., Pesta, B. J., Francis, G., & Kirkegaard E. (2023). International meta-analysis of differential fertility for intelligence. Retrieved from https://openpsych.net/files/submissions/9_International_meta-analysis_of_differential_fertility_for_intelligence.pdf
Worldometer (2022). GDP per Capita. worldometers. Retrieved from http://web.archive.org/web/20240421104059/https://www.worldometers.info/gdp/gdp-per-capita/
Eurostat (2023). Industrial Production Statistics. Eurostat | Statistics Explained. Retrieved from https://ec.europa.eu/eurostat/statistics-explained/SEPDF/cache/7316.pdf
Spolaore, E., & Wacziarg, R. (2022). Fertility and modernity. The Economic Journal, 132(642), 796-833. Retrieved from https://www.nber.org/system/files/working_papers/w25957/w25957.pdf
Clark, G. (2007). A Farewell To Alms. Princeton University Press. Retrieved from https://not-equal.org/content/pdf/misc/Clark2007.pdf
McEvoy, O. (2023). Total fertility rate in Europe 2023, by country. Statista. Retrieved from https://www.statista.com/statistics/612074/fertility-rates-in-european-countries/
Van der Linde, D., Konings, E. E. M., Slager, M. A., Witsenburg, M., Helbing, W. A., Takkenberg, J. J. M., & Roos-Hesselink, J. W. (2011). Birth Prevalence of Congenital Heart Disease Worldwide. Journal of the American College of Cardiology, 58(21), 2241–2247. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.jacc.2011.08.025
Zhao, L., Chen, L., Yang, T., Wang, T., Zhang, S., Chen, L., … Qin, J. (2020). Birth prevalence of congenital heart disease in China, 1980–2019: a systematic review and meta-analysis of 617 studies. European Journal of Epidemiology 31, 631-642. Retrieved from https://sci-hub.ru/https://doi.org/10.1007/s10654-020-00653-0
Khairy, P., Ionescu-Ittu, R., Mackie, A. S., Abrahamowicz, M., Pilote, L., & Marelli, A. J. (2010). Changing Mortality in Congenital Heart Disease. Journal of the American College of Cardiology, 56(14), 1149–1157. Retrieved from https://sci-hub.ru/https:/doi.org/10.1016/j.jacc.2010.03.085
Zimmerman, M. S., Smith, A. G. C., Sable, C. A., Echko, M. M., Wilner, L. B., Olsen, H. E., ... & Kassebaum, N. J. (2020). Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet Child & Adolescent Health, 4(3), 185-200. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/S2352-4642(19)30402-X
Twenge, J. M., Sherman, R. A., & Wells, B. E. (2016). Changes in American Adults’ Reported Same-Sex Sexual Experiences and Attitudes, 1973–2014. Archives of Sexual Behavior, 45(7), 1713–1730. Retrieved from https://sci-hub.ru/https://doi.org/10.1007/s10508-016-0769-4
Papadatou-Pastou, M., Ntolka, E., Schmitz, J., Martin, M., Munafò, M. R., Ocklenburg, S., & Paracchini, S. (2020). Human handedness: A meta-analysis. Psychological bulletin, 146(6), 481. Retrieved from https://not-equal.org/content/pdf/misc/10.1037.bul0000229.pdf
Lerner, A., Jeremias, P., & Matthias, T. (2015). The world incidence and prevalence of autoimmune diseases is increasing. Int J Celiac Dis, 3(4), 151-5. Retrieved from https://not-equal.org/content/pdf/misc/Lerner2015.pdf
Conrad, N., Misra, S., Verbakel, J. Y., Verbeke, G., Molenberghs, G., Taylor, P. N., ... & Cambridge, G. (2023). Incidence, prevalence, and co-occurrence of autoimmune disorders over time and by age, sex, and socioeconomic status: a population-based cohort study of 22 million individuals in the UK. The Lancet, 401(10391), 1878-1890. Retrieved from https://not-equal.org/content/pdf/misc/Conrad2023.pdf
King, J. A., Jeong, J., Underwood, F. E., Quan, J., Panaccione, N., Windsor, J. W., … Kaplan, G. G. (2020). Incidence of Celiac Disease Is Increasing Over Time. The American Journal of Gastroenterology, 115(4), 507–525. Retrieved from https://sci-hub.ru/https://doi.org/10.14309/ajg.0000000000000523
Sýkora, J., Pomahačová, R., Kreslová, M., Cvalínová, D., Štych, P., & Schwarz, J. (2018). Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World Journal of Gastroenterology, 24(25), 2741–2763. Retrieved from https://sci-hub.ru/https:/doi.org/10.3748/wjg.v24.i25.2741
Barnes, E. L., Kochar, B., Jessup, H. R., & Herfarth, H. H. (2019). The Incidence and Definition of Crohn’s Disease of the Pouch: A Systematic Review and Meta-analysis. Inflammatory Bowel Diseases, 25(9), 1474–1480. Retrieved from https://sci-hub.ru/https://doi.org/10.1093/ibd/izz005
West, J., Fleming, K. M., Tata, L. J., Card, T. R., & Crooks, C. J. (2014). Incidence and Prevalence of Celiac Disease and Dermatitis Herpetiformis in the UK Over Two Decades: Population-Based Study. The American Journal of Gastroenterology, 109(5), 757–768. Retrieved from https://sci-hub.ru/https:/doi.org/10.1038/ajg.2014.55
Weström, L. (1980). Incidence, prevalence, and trends of acute pelvic inflammatory disease and its consequences in industrialized countries. American Journal of Obstetrics and Gynecology, 138(7), 880–892. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/0002-9378(80)91077-7
Bach, J.-F. (2002). The Effect of Infections on Susceptibility to Autoimmune and Allergic Diseases. New England Journal of Medicine, 347(12), 911–920. Retrieved from https://sci-hub.ru/https:/doi.org/10.1056/NEJMra020100
Lerner, A., & Matthias, T. (2015). Changes in intestinal tight junction permeability associated with industrial food additives explain the rising incidence of autoimmune disease. Autoimmunity Reviews, 14(6), 479–489. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.autrev.2015.01.009
Vancamelbeke, M., & Vermeire, S. (2017). The intestinal barrier: a fundamental role in health and disease. Expert Review of Gastroenterology & Hepatology, 11(9), 821–834. Retrieved from https://sci-hub.ru/https://doi.org/10.1080/17474124.2017.1343143
Askari, G., Ghavami, A., Shahdadian, F., & Moravejolahkami, A. R. (2021). Effect of synbiotics and probiotics supplementation on autoimmune diseases: A systematic review and meta-analysis of clinical trials. Clinical Nutrition, 40(5), 3221–3234. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.clnu.2021.02.015
Zeng, L., Deng, Y., Yang, K., Chen, J., He, Q., & Chen, H. (2022). Safety and efficacy of fecal microbiota transplantation for autoimmune diseases and autoinflammatory diseases: A systematic review and meta-analysis. Frontiers in Immunology, 13(944387), 1-22. Retrieved from https://not-equal.org/content/pdf/misc/Zeng2022.pdf
Doucet, M., Rochette, L., & Hamel, D. (2016). Incidence, prevalence, and mortality trends in chronic obstructive pulmonary disease over 2001 to 2011: a public health point of view of the burden. Canadian respiratory journal, 2016. Article ID:7518287. Retrieved from https://sci-hub.ru/https://doi.org/10.1155/2016/7518287
Gershon, A. S. (2010). Trends in Chronic Obstructive Pulmonary Disease Prevalence, Incidence, and Mortality in Ontario, Canada, 1996 to 2007. Archives of Internal Medicine, 170(6), 560. Retrieved from https://sci-hub.ru/https:/doi.org/10.1001/archinternmed.2010.17
Xie, M., Liu, X., Cao, X., Guo, M., & Li, X. (2020). Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respiratory Research, 21(1). Retrieved from https://sci-hub.ru/https:/doi.org/10.1186/s12931-020-1291-8
Liu, L., He, W., Zhu, J., Deng, K., Tan, H., Xiang, L., ... & Li, X. (2023). Global prevalence of congenital hypothyroidism among neonates from 1969 to 2020: a systematic review and meta-analysis. European Journal of Pediatrics, 182(7), 2957-2965. Retrieved from https://not-equal.org/content/pdf/misc/10.1007.s00431-023-04932-2.pdf
Kaiserman, I., Maytal, A., Siebner, R., & Sack, J. (1997). Effects of immigration on the incidence of congenital hypothyroidism. European journal of endocrinology, 137(4), 356-359. Retrieved from https://sci-hub.ru/https://doi.org/10.1530/eje.0.1370356
Barry, Y., Bonaldi, C., Goulet, V., Coutant, R., Léger, J., Paty, A. C., ... & Roussey, M. (2016). Increased incidence of congenital hypothyroidism in France from 1982 to 2012: a nationwide multicenter analysis. Annals of Epidemiology, 26(2), 100-105. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.annepidem.2015.11.005
Park, K. S. (2021). Analysis of worldwide carrier frequency and predicted genetic prevalence of autosomal recessive congenital hypothyroidism based on a general population database. Genes, 12(6), 863. Retrieved from https://sci-hub.ru/https://doi.org/10.3390/genes12060863
Brix, T. H., & Hegedüs, L. (2011, April). Twins as a tool for evaluating the influence of genetic susceptibility in thyroid autoimmunity. In Annales d'endocrinologie (Vol. 72, No. 2, pp. 103-107). Elsevier Masson. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.ando.2011.03.013
Makretskaya, N., Bezlepkina, O., Kolodkina, A., Kiyaev, A., Vasilyev, E. V., Petrov, V., … Tiulpakov, A. (2018). High frequency of mutations in “dyshormonogenesis genes” in severe congenital hypothyroidism. PLOS ONE, 13(9), e0204323. Retrieved from https://sci-hub.ru/https://doi.org/10.1371/journal.pone.0204323
Albert, B. B., Cutfield, W. S., Webster, D., Carll, J., Derraik, J. G. B., Jefferies, C., … Hofman, P. L. (2012). Etiology of Increasing Incidence of Congenital Hypothyroidism in New Zealand from 1993–2010. The Journal of Clinical Endocrinology & Metabolism, 97(9), 3155–3160. Retrieved from https://sci-hub.ru/https://doi.org/10.1210/jc.2012-1562
Hinton, C. F., Harris, K. B., Borgfeld, L., Drummond-Borg, M., Eaton, R., Lorey, F., ... & Pass, K. A. (2010). Trends in incidence rates of congenital hypothyroidism related to select demographic factors: data from the United States, California, Massachusetts, New York, and Texas. Pediatrics, 125(Supplement_2), S37-S47. Retrieved from https://sci-hub.ru/https://doi.org/10.1542/peds.2009-1975D
Spear, M. L., Diaz-Papkovich, A., Ziv, E., Yracheta, J. M., Gravel, S., Torgerson, D. G., & Hernandez, R. D. (2020). Recent shifts in the genomic ancestry of Mexican Americans may alter the genetic architecture of biomedical traits. Elife, 9, e56029. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7771964/pdf/elife-56029.pdf
Deladoëy, J., Ruel, J., Giguère, Y., & Van Vliet, G. (2011). Is the Incidence of Congenital Hypothyroidism Really Increasing? A 20-Year Retrospective Population-Based Study in Québec. The Journal of Clinical Endocrinology & Metabolism, 96(8), 2422–2429. Retrieved from https://sci-hub.ru/https://doi.org/10.1210/jc.2011-1073
McGrath, N., Hawkes, C. P., McDonnell, C. M., Cody, D., O’Connell, S. M., Mayne, P. D., & Murphy, N. P. (2018). Incidence of congenital hypothyroidism over 37 years in Ireland. Pediatrics, 142(4). Retrieved from https://sci-hub.ru/https://doi.org/10.1542/peds.2018-1199
Liu, L., He, W., Zhu, J., Deng, K., Tan, H., Xiang, L., ... & Li, X. (2023). Global prevalence of congenital hypothyroidism among neonates from 1969 to 2020: a systematic review and meta-analysis. European Journal of Pediatrics, 182(7), 2957-2965. Retrieved from https://not-equal.org/content/pdf/misc/10.1007.s00431-023-04932-2.pdf
Said, W. P., Arto, K. S., Pratita, W., & Sufitni, S. (2023). Intelligence quotient (IQ) outcome in children with early-treated congenital hypothyroidism: a systematic review and meta-analysis. Paediatrica Indonesiana, 63(4), 290-7. Retrieved from https://not-equal.org/content/pdf/misc/10.14238.pi63.4.2023.290-7.pdf
Danner, E., Niuro, L., Huopio, H., Niinikoski, H., Viikari, L., Kero, J., & Jääskeläinen, J. (2023). Incidence of primary congenital hypothyroidism over 24 years in Finland. Pediatric Research, 93(3), 649-653. Retrieved from https://sci-hub.ru/https://doi.org/10.1038/s41390-022-02118-4
Gao, S., Burney, H. N., Callahan, C. M., Purnell, C. E., & Hendrie, H. C. (2019). Incidence of dementia and Alzheimer disease over time: A meta‐analysis. Journal of the American Geriatrics Society, 67(7), 1361-1369. Retrieved from https://sci-hub.ru/https://doi.org/10.1111/jgs.16027
Wu, Y. T., Beiser, A. S., Breteler, M. M., Fratiglioni, L., Helmer, C., Hendrie, H. C., ... & Brayne, C. (2017). The changing prevalence and incidence of dementia over time—current evidence. Nature Reviews Neurology, 13(6), 327-339. Retrieved from https://sci-hub.ru/https://doi.org/10.1038/nrneurol.2017.63
Savica, R., Grossardt, B. R., Bower, J. H., Ahlskog, J. E., & Rocca, W. A. (2016). Time trends in the incidence of Parkinson disease. JAMA neurology, 73(8), 981-989. Retrieved from https://sci-hub.ru/https:/doi.org/10.1001/jamaneurol.2016.0947
Rees, F., Doherty, M., Grainge, M. J., Lanyon, P., & Zhang, W. (2017). The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology, 56(11), 1945-1961. Retrieved from https://sci-hub.ru/https://doi.org/10.1093/rheumatology/kex260
Lane, J., Ng, H. S., Poyser, C., Lucas, R. M., & Tremlett, H. (2022). Multiple sclerosis incidence: A systematic review of change over time by geographical region. Multiple Sclerosis and Related Disorders, 63, 103932. Retrieved from https://not-equal.org/content/pdf/misc/Lane2022.pdf
A. Caldwell, J., Knapik, J. J., & Lieberman, H. R. (2017). Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. Journal of sleep research, 26(5), 665-670. Retrieved from https://sci-hub.ru/https://doi.org/10.1111/jsr.12543
Zhang, Y., Luo, G., Li, M., Guo, P., Xiao, Y., Ji, H., & Hao, Y. (2019). Global patterns and trends in ovarian cancer incidence: age, period and birth cohort analysis. BMC cancer, 19, 1-14. Retrieved from https://sci-hub.ru/https:/doi.org/10.1186/s12885-019-6139-6
Barnholtz-Sloan, J. S., Maldonado, J. L., Pow-Sang, J., & Guiliano, A. R. (2007, September). Incidence trends in primary malignant penile cancer. In Urologic Oncology: Seminars and Original Investigations (Vol. 25, No. 5, pp. 361-367). Elsevier. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.urolonc.2006.08.029
Deng, X., Liu, Y., Zhan, X., Chen, T., Jiang, M., Jiang, X., ... & Fu, B. (2022). Trends in incidence, mortality, and survival of penile cancer in the United States: A population-based study. Frontiers in Oncology, 12, 891623. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9248743/pdf/fonc-12-891623.pdf
Ansa, B., Coughlin, S., Alema-Mensah, E., & Smith, S. (2018). Evaluation of Colorectal Cancer Incidence Trends in the United States (2000–2014). Journal of Clinical Medicine, 7(2), 22. Retrieved from https://sci-hub.ru/https://doi.org/10.3390/jcm7020022
Cheng, L., Eng, C., Nieman, L. Z., Kapadia, A. S., & Du, X. L. (2011). Trends in colorectal cancer incidence by anatomic site and disease stage in the United States from 1976 to 2005. American journal of clinical oncology, 34(6), 573-580. Retrieved from https://sci-hub.ru/https:/doi.org/10.1097/COC.0b013e3181fe41ed
Guy Jr, G. P., Thomas, C. C., Thompson, T., Watson, M., Massetti, G. M., Richardson, L. C., & Centers for Disease Control and Prevention (CDC). (2015). Vital signs: melanoma incidence and mortality trends and projections—United States, 1982–2030. MMWR Morb Mortal Wkly Rep, 64(21), 591-596. Retrieved from https://www.cdc.gov/mmwr/pdf/wk/mm6421.pdf
Liu, Z., Jiang, Y., Yuan, H., Fang, Q., Cai, N., Suo, C., ... & Chen, X. (2019). The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. Journal of hepatology, 70(4), 674-683. Retrieved from https://not-equal.org/content/pdf/misc/Zhenqiu2018.pdf
Du, M., Nair, R., Jamieson, L., Liu, Z., & Bi, P. (2020). Incidence trends of lip, oral cavity, and pharyngeal cancers: global burden of disease 1990–2017. Journal of dental research, 99(2), 143-151. Retrieved from https://sci-hub.ru/https://doi.org/10.1177/0022034519894963
Protzko, J. (2020). Kids These Days! Increasing delay of gratification ability over the past 50 years in children. Intelligence, 80, 101451. Retrieved from https://sci-hub.ru/https:/doi.org/10.1016/j.intell.2020.101451
Recueil, C. (2023). Age, Crime, and their Weakening Link. Cremieux Receuil. Retrieved from https://cremieux.xyz/p/age-crime-and-their-weakening-link
Strizek, J., Uhl, A., Schaub, M., & Malischnig, D. (2021). Alcohol and cigarette use among adolescents and young adults in Austria from 2004–2020: Patterns of change and associations with socioeconomic variables. International Journal of Environmental Research and Public Health, 18(24), 13080. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8701464/pdf/ijerph-18-13080.pdf
Saad, L. (2023). Young Adults in U.S. Drinking Less Than in Prior Decades. Gallup News. Retrieved from https://news.gallup.com/poll/509690/young-adults-drinking-less-prior-decades.aspx
Lei, L., & South, S. J. (2024). The COVID-19 Pandemic and Sexual Activity Among Young Adults. Population Research and Policy Review, 43(2), 17. Retrieved from https://not-equal.org/content/pdf/misc/Lei2023.pdf
Alexander (2023). Are 27% Of Young Men Really Virgins? (And Why). datepsych. Retrieved from https://datepsychology.com/are-27-of-young-men-really-virgins-and-why/
Trialists’Collaboration, B. P. L. T., Ying, A., Arima, H., Czernichow, S., Woodward, M., Huxley, R., ... & Neal, B. (2015). Effects of blood pressure lowering on cardiovascular risk according to baseline body-mass index: a meta-analysis of randomised trials. Lancet, 385(9971), 867-74. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/S0140-6736(14)61171-5
Roulet, C., Bovet, P., Brauchli, T., Simeoni, U., Xi, B., Santschi, V., ... & Chiolero, A. (2017). Secular trends in blood pressure in children: a systematic review. The Journal of Clinical Hypertension, 19(5), 488-497. Retrieved from https://sci-hub.ru/https://doi.org/10.1111/jch.12955
Ferrari, A. J., Stockings, E., Khoo, J. P., Erskine, H. E., Degenhardt, L., Vos, T., & Whiteford, H. A. (2016). The prevalence and burden of bipolar disorder: findings from the Global Burden of Disease Study 2013. Bipolar disorders, 18(5), 440-450. Retrieved from https://sci-hub.ru/https://doi.org/10.1111/bdi.12423
Schürmann, J., & Margraf, J. (2018). Age of anxiety and depression revisited: A meta-analysis of two European community samples (1964-2015). International Journal of Clinical and Health Psychology, 18(2), 102–112. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.ijchp.2018.02.002
Alicandro, G., Malvezzi, M., Gallus, S., La Vecchia, C., Negri, E., & Bertuccio, P. (2019). Worldwide trends in suicide mortality from 1990 to 2015 with a focus on the global recession time frame. International Journal of Public Health, 64(5), 785–795. Retrieved from https://sci-hub.ru/https://doi.org/10.1007/s00038-019-01219-y
Thomas, K., & Gunnell, D. (2010). Suicide in England and Wales 1861–2007: a time-trends analysis. International Journal of Epidemiology, 39(6), 1464-1475. Retrieved from https://sci-hub.ru/https://doi.org/10.1093/ije/dyq094
Kirkegaard, E. (2024). Autism diagnoses are rising, yes, but autism, probably not. Emil Kirkegaard Things. Retrieved from https://emilkirkegaard.com/p/autism-diagnoses-are-rising-yes-but
Rose, L., McKim, D., Leasa, D., Nonoyama, M., Tandon, A., Bai, Y. Q., ... & Gershon, A. (2019). Trends in incidence, prevalence, and mortality of neuromuscular disease in Ontario, Canada: a population-based retrospective cohort study (2003-2014). PloS one, 14(3), e0210574. Retrieved from https://sci-hub.ru/https://doi.org/10.1371/journal.pone.0210574
Cea-Soriano, L., Fowkes, F. G. R., Johansson, S., Allum, A. M., & Rodriguez, L. A. G. (2018). Time trends in peripheral artery disease incidence, prevalence and secondary preventive therapy: a cohort study in The Health Improvement Network in the UK. BMJ open, 8(1), e018184. Retrieved from https://sci-hub.ru/https://doi.org/10.1136/bmjopen-2017-018184
Erdal, B. S., Clymer, B. D., Yildiz, V. O., Julian, M. W., & Crouser, E. D. (2012). Unexpectedly high prevalence of sarcoidosis in a representative US Metropolitan population. Respiratory medicine, 106(6), 893-899. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.rmed.2012.02.007
Dana, R., Bradley, J. L., Guerin, A., Pivneva, I., Stillman, I. Ö., Evans, A. M., & Schaumberg, D. A. (2019). Estimated prevalence and incidence of dry eye disease based on coding analysis of a large, all-age United States health care system. American journal of ophthalmology, 202, 47-54. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.ajo.2019.01.026
Eun-Jin, L., Ahn, Y. C., Eun-Su, J., Si-Woo, L., Su-Hwa, L., & Chang-Gue, S. (2020). Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). Journal of Translational Medicine, 18, 1. Retrieved from https://sci-hub.ru/https://doi.org/10.1186/s12967-020-02269-0
Andrews, P., Steultjens, M., & Riskowski, J. (2018). Chronic widespread pain prevalence in the general population: a systematic review. European Journal of Pain, 22(1), 5-18. Retrieved from https://sci-hub.ru/https://doi.org/10.1002/ejp.1090
Hugoson, A., Sjödin, B., & Norderyd, O. (2008). Trends over 30 years, 1973–2003, in the prevalence and severity of periodontal disease. Journal of clinical periodontology, 35(5), 405-414. Retrieved from https://sci-hub.ru/https://doi.org/10.1111/j.1600-051X.2008.01225.x
Magliano, D. J., Islam, R. M., Barr, E. L., Gregg, E. W., Pavkov, M. E., Harding, J. L., ... & Shaw, J. E. (2019). Trends in incidence of total or type 2 diabetes: systematic review. bmj, 366. Retrieved from https://sci-hub.ru/https://doi.org/10.1136/bmj.l5003
Nolen, L., Haberling, D., Scollard, D., Truman, R., Rodriguez-Lainz, A., Blum, L., & Blaney, D. (2014). Incidence of Hansen’s disease—United States, 1994–2011. MMWR Morb Mortal Wkly Rep, 63(43), 969-972. Retrieved from https://www.cdc.gov/mmwr/pdf/wk/mm6343.pdf
Anderson, E. L., Howe, L. D., Jones, H. E., Higgins, J. P. T., Lawlor, D. A., & Fraser, A. (2015). The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLOS ONE, 10(10), e0140908. Retrieved from https://sci-hub.ru/https://doi.org/10.1371/journal.pone.0140908
Akushevich, I., Kravchenko, J., Ukraintseva, S., Arbeev, K., & Yashin, A. I. (2013). Time trends of incidence of age-associated diseases in the US elderly population: Medicare-based analysis. Age and ageing, 42(4), 494-500. Retrieved from https://sci-hub.ru/https://doi.org/10.1093/ageing/aft032
Kawatkar, A. A., Gabriel, S. E., & Jacobsen, S. J. (2019). Secular trends in the incidence and prevalence of rheumatoid arthritis within members of an integrated health care delivery system. Rheumatology International, 39, 541-549. Retrieved from https://sci-hub.ru/https://doi.org/10.1007/s00296-018-04235-y
Edvardsson, V. O., Indridason, O. S., Haraldsson, G., Kjartansson, O., & Palsson, R. (2013). Temporal trends in the incidence of kidney stone disease. Kidney international, 83(1), 146-152. Retrieved from https://sci-hub.ru/https://doi.org/10.1038/ki.2012.320
Emdin, C. A., Anderson, S. G., Woodward, M., & Rahimi, K. (2015). Usual Blood Pressure and Risk of New-Onset Diabetes. Journal of the American College of Cardiology, 66(14), 1552–1562. Retrieved from https://sci-hub.ru/https:/doi.org/10.1016/j.jacc.2015.07.059
Cai, L., Wu, Y., Wilson, R. F., Segal, J. B., Kim, M. T., & Wang, Y. (2014). Effect of Childhood Obesity Prevention Programs on Blood Pressure: A Systematic Review and Meta-Analysis. Circulation, 129(18), 1832–1839. Retrieved from https://sci-hub.ru/https:/doi.org//10.1161/CIRCULATIONAHA.113.005666
Neter, J. E., Stam, B. E., Kok, F. J., Grobbee, D. E., & Geleijnse, J. M. (2003). Influence of Weight Reduction on Blood Pressure: A Meta-Analysis of Randomized Controlled Trials. Hypertension, 42(5), 878–884. Retrieved from https://sci-hub.ru/https:/doi.org/10.1161/01.HYP.0000094221.86888.AE
Abdullah, A., Peeters, A., de Courten, M., & Stoelwinder, J. (2010). The magnitude of association between overweight and obesity and the risk of diabetes: A meta-analysis of prospective cohort studies. Diabetes Research and Clinical Practice, 89(3), 309–319. Retrieved from https://sci-hub.ru/https://doi.org/10.1016/j.diabres.2010.04.012
Bell, J. A., Kivimaki, M., & Hamer, M. (2014). Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obesity Reviews, 15(6), 504–515. Retrieved from https://sci-hub.ru/https:/doi.org/10.1111/obr.12157
Offer, A. (2001). Body Weight and Self-Control in the United States and Britain since the 1950s. Social History of Medicine, 14(1), 79–106. Retrieved from https://sci-hub.ru/https://doi.org/10.1093/shm/14.1.79
Ogden, C. L., Carroll, M. D., Lawman, H. G., Fryar, C. D., Kruszon-Moran, D., Kit, B. K., & Flegal, K. M. (2016). Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988-1994 Through 2013-2014. JAMA, 315(21), 2292. Retrieved from https://sci-hub.ru/https:/doi.org/10.1001/jama.2016.6361
Juul, F., & Hemmingsson, E. (2015). Trends in consumption of ultra-processed foods and obesity in Sweden between 1960 and 2010. Public Health Nutrition, 18(17), 3096–3107. Retrieved from https://sci-hub.ru/https://doi.org/10.1017/S1368980015000506
Garrido-Miguel, M., Cavero-Redondo, I., Álvarez-Bueno, C., Rodríguez-Artalejo, F., Moreno, L. A., Ruiz, J. R., … Martínez-Vizcaíno, V. (2019). Prevalence and Trends of Overweight and Obesity in European Children From 1999 to 2016. JAMA Pediatrics, 173(10), e192430. Retrieved from https://sci-hub.ru/https:/doi.org/10.1001/jamapediatrics.2019.2430
Hellermann, J. P. (2003). Incidence of Heart Failure after Myocardial Infarction: Is It Changing over Time? American Journal of Epidemiology, 157(12), 1101–1107. Retrieved from https://sci-hub.ru/https://doi.org/10.1093/aje/kwg078
Sidney, S., Quesenberry, C. P., Jaffe, M. G., Sorel, M., Nguyen-Huynh, M. N., Kushi, L. H., … Rana, J. S. (2016). Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiology, 1(5), 594. Retrieved from https://sci-hub.ru/https:/doi.org/10.1001/jamacardio.2016.1326
Yang, Q., Cogswell, M. E., Flanders, W. D., Hong, Y., Zhang, Z., Loustalot, F., … Hu, F. B. (2012). Trends in Cardiovascular Health Metrics and Associations With All-Cause and CVD Mortality Among US Adults. JAMA, 307(12), 1273. Retrieved from https://sci-hub.ru/https:/doi.org/10.1001/jama.2012.339
Shin, M. E., & McCarthy, W. J. (2013). The association between county political inclination and obesity: Results from the 2012 presidential election in the United States. Preventive Medicine, 57(5), 721–724. Retrieved from https://sci-hub.ru/https:/doi.org/10.1016/j.ypmed.2013.07.026
Weir, H. K., Thompson, T. D., Soman, A., Møller, B., & Leadbetter, S. (2015). The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer, 121(11), 1827-1837. Retrieved from https://sci-hub.ru/https:/doi.org/10.1002/cncr.29258


























Good effort post!
I have a few comments regarding the section on impulse control, while technically what you cited isn't wrong, I find some of its implications a bit misleading. For instance, wouldn't the graph detailing weakening impulsivity exclusivity towards younger age cohorts be proof of a widening (more prevalent) trend? Also the studies cited that provide evidence for decreased drinking and smoking don't provide data like increases in cannabis and nicotine use in younger demographics which would contextualise their findings. As for casual sex, worsening social skills for younger generations could be a factor, as well as declining T levels that would have men appear younger and less sexually attractive towards women who would want to engage in such recreational activities, unless were talking about prostitution of course, although given how little data I could find on it, this is probably not the case lol.